Chronic Pancreatitis - Expert Diagnosis & Management
Chronic Pancreatitis
Understanding and Managing Chronic Pancreatitis
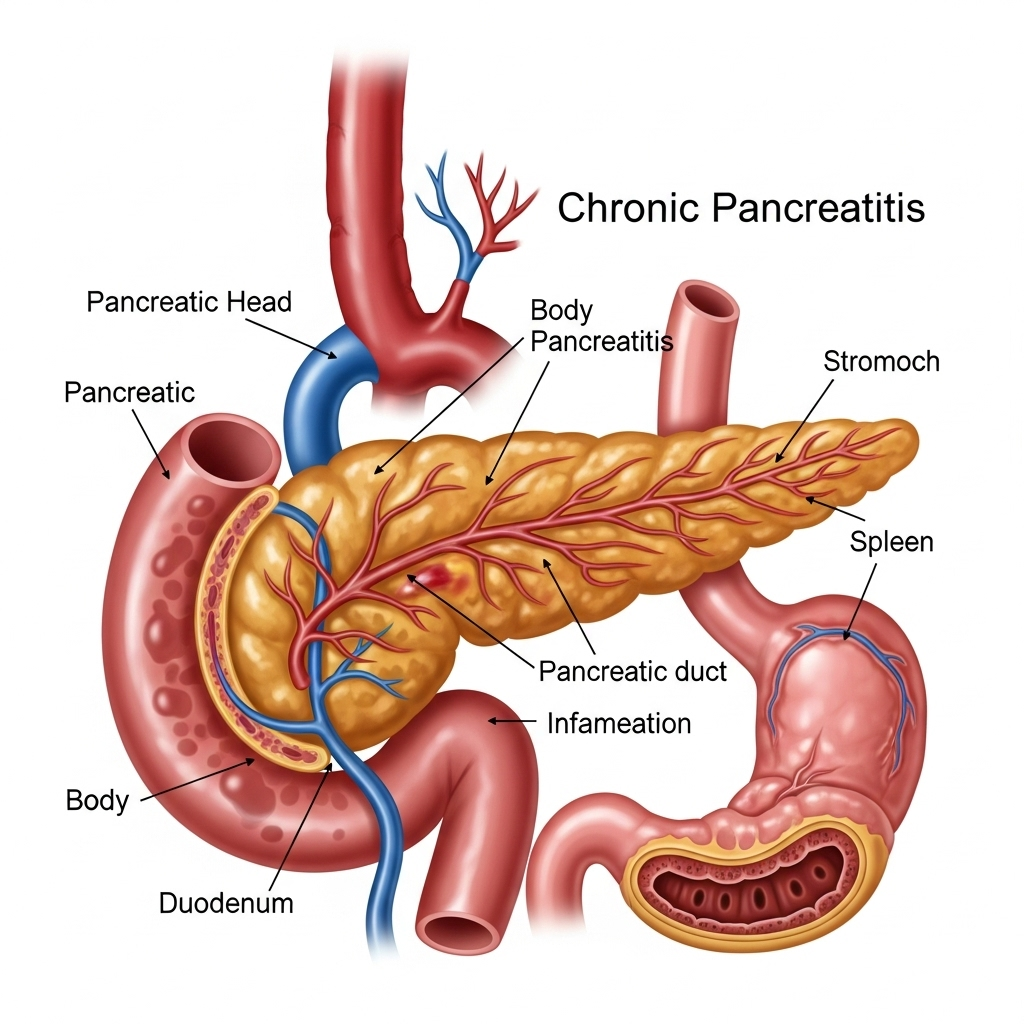
Chronic pancreatitis is a progressive inflammatory disease of the pancreas that leads to irreversible damage and loss of its normal function. Unlike acute pancreatitis, which is a sudden inflammation, chronic pancreatitis develops over time and can cause persistent pain, maldigestion, and eventually diabetes.
What is Chronic Pancreatitis?
The pancreas is a vital organ located behind the stomach that produces enzymes essential for digestion (exocrine function) and hormones like insulin for blood sugar regulation (endocrine function). In chronic pancreatitis, repeated inflammation or damage to the pancreas results in scarring and fibrosis, which impairs its ability to produce these enzymes and hormones. This leads to digestive problems and, in many cases, diabetes.
Common Causes:
While the exact cause can sometimes be unknown (idiopathic), common factors contributing to chronic pancreatitis include:
- Alcohol Abuse: This is the most common cause, especially with long-term heavy consumption.
- Genetic Factors: Certain gene mutations can increase susceptibility.
- Autoimmune Diseases: The body's immune system mistakenly attacks the pancreas.
- Ductal Obstruction: Blockages in the pancreatic duct due to stones, tumors, or strictures.
- Cystic Fibrosis: A genetic disorder that affects mucus production, including in the pancreas.
- Severe Hypertriglyceridemia: Very high levels of triglycerides in the blood.
- Recurrent Acute Pancreatitis: Repeated bouts of acute inflammation can lead to chronic changes.
Symptoms of Chronic Pancreatitis:
Symptoms often develop gradually and can vary in intensity. They typically include:
- Abdominal Pain: Persistent or recurrent pain, often severe, in the upper abdomen that may radiate to the back. It can worsen after eating.
- Maldigestion: Due to insufficient digestive enzymes, leading to:
- Steatorrhea: Fatty, foul-smelling stools that are difficult to flush.
- Weight Loss: Despite maintaining normal eating habits, due to poor nutrient absorption.
- Nausea and Vomiting: Especially during painful episodes.
- Diabetes: As the insulin-producing cells are damaged, leading to elevated blood sugar levels.
- Jaundice: If the bile duct becomes obstructed.
Diagnosis:
Diagnosing chronic pancreatitis involves a comprehensive approach:
- Medical History and Physical Exam: Dr. Dhar will thoroughly assess your symptoms, lifestyle, and medical background.
- Blood Tests: To check for elevated pancreatic enzymes (amylase, lipase, though often normal in chronic cases), blood sugar levels, and nutritional deficiencies.
- Stool Tests: To measure fat content, indicating malabsorption.
- Imaging Tests:
- CT Scan or MRI: To visualize the pancreas, detect calcifications, ductal changes, or pseudocysts.
- Endoscopic Ultrasound (EUS): A highly sensitive test to detect subtle changes in the pancreas and biopsy suspicious lesions.
- MRCP (Magnetic Resonance Cholangiopancreatography): A specialized MRI to visualize the bile and pancreatic ducts.
- ERCP (Endoscopic Retrograde Cholangiopancreatography): Used for both diagnosis and therapeutic interventions, such as removing stones or placing stents in obstructed ducts.
Treatment and Management:
The goal of chronic pancreatitis treatment is to manage pain, improve digestion, prevent complications, and treat any underlying causes. Dr. Neeraj Dhar provides a personalized, multi-faceted treatment plan that may include:
- Pain Management: Tailored strategies including medications, and in some cases, nerve blocks or endoscopic procedures (e.g., stenting or stone removal via ERCP).
- Pancreatic Enzyme Replacement Therapy (PERT): Oral enzyme supplements to help with digestion and reduce malabsorption and steatorrhea.
- Dietary Modifications: A low-fat diet, frequent small meals, and avoiding alcohol are crucial. Nutritional counseling may be provided.
- Diabetes Management: If diabetes develops, insulin therapy or other diabetes medications will be prescribed.
- Endoscopic Interventions: Dr. Dhar uses advanced endoscopic techniques like ERCP to remove stones from pancreatic ducts, dilate strictures, or drain pseudocysts.
- Surgical Consultation: In cases of intractable pain, severe complications, or ductal obstruction not amenable to endoscopy, surgical options may be considered.
- Lifestyle Changes: Quitting smoking and strict avoidance of alcohol are paramount for preventing further damage.
Why Choose Dr. Neeraj Dhar for Chronic Pancreatitis?
Dr. Neeraj Dhar is a highly experienced Gastroenterologist in Faridabad, specializing in the comprehensive diagnosis and management of complex pancreatic diseases, including chronic pancreatitis. His expertise in advanced endoscopic procedures like ERCP and EUS is critical for both accurate diagnosis and effective therapeutic interventions for chronic pancreatitis. Dr. Dhar emphasizes a patient-centric approach, focusing on alleviating symptoms, improving quality of life, and preventing disease progression through evidence-based treatments and continuous patient education.
If you or a loved one are experiencing symptoms suggestive of chronic pancreatitis, or seeking advanced management for an existing diagnosis, consult Dr. Neeraj Dhar for expert care and a compassionate approach to your digestive health.
